Final year general medicine long case presentation
Bhavani vegesena
Roll no 141
Saturday, June 11, 2022
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever
CASE
A 19 year old male student came to the opd with the chief complaints of :
1.shortness of breath since 10 days ,
2.fever since 10 days ,
3.cough since 3 days
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 15 days back , then he developed shortness of breath on mild exercise like walking up the stairs for which he went to nalgonda government hospital after which it subsided on treatment.
10 days ago he had another episode of shortness of breath which was associated with fever. The patient was referred to our hospital for further treatment.
The fever was sudden in onset , intermittent , low grade , not associated with chills and rigors and no evening rise of temperature.
The patient had cough since 3 days which was non productive which was relieved on medication
There was no history of palpitations , orthopnea, paroxysmal nocturnal dyspnoea.
There is a history of loss of weight of about 5 kg in 2months
No complaints of chest pain , hemoptysis.
PAST HISTORY :
No history of similar complains in the past.
No history of TB , diabetes , hypertension , bronchial asthma and epilepsy.
FAMILY HISTORY :
No history of similar complaints in the family
PERSONAL HISTORY :
Appetite : Normal
Diet : Mixed
Sleep : Adequate
Bowel and bladder movements : Normal
No addictions and no drug allergies
Occupation : Student
DAILY ROUTINE OF THE PATIENT :
The patient is student by occupation. He lives in a hostel in Hyderabad and is currently pursuing his B.Tech degree.
A usual day in his life:
He is an active person and frequently plays sports.GENERAL EXAMINATION :
Patient is conscious , coherent and cooperative, moderately built and nourished and well oriented to time , place and person.
Pallor - Absent
Icterus - Absent
Clubbing - Absent
Cyanosis - Absent
Lymphadenopathy - Absent
Edema - Absent
VITALS :
Temperature : Febrile
Pulse : 98 beats per minute
Respiratory rate : 16 cycles per minute
Blood pressure : 120/85 mm of Hg
SYSTEMIC EXAMINATION :
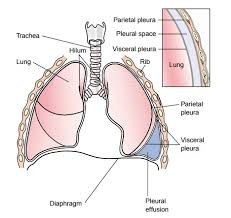
RESPIRATORY SYSTEM :
INSPECTION :
Shape of the chest : elliptical
Symmetry : bilaterally symmetrical
Trachea : Central in position
Expansion of the chest : Decreased on left side
Accessory muscles use for respiration : Not present
Type of respiration : Abdomino thoracic
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulders
Right sided supraclavicular , infraclavicular hollow present
No crowding of ribs
Spinoscapular distance equal on both sides
PALPATION :
All inspectory findings are confirmed
No local rise of temperature
No tenderness
Trachea deviated to right side
Anteroposterior diameter- 21cm
Transverse diameter-30cm
Ratio: AP/T- 0.7
Chest expansion: 2.5 cm
Chest movements decreased on left side
Tactile vocal Fremitus decreased on left infra scapular area
Vocal resonance decreased on left infra scapular area
Video of examination of chest expansion
PERCUSSION :
Left :
Direct : dull
Indirect : dull
Liver dullness for right 5th intercostal space
Cardiac dullness within normal limits
AUSCULTATION :
Bilateral air entry present
Normal vesicular breath sounds heard
Decreased intensity of breath sounds in left InfraMammaryArea , InfraAxillaryArea .
Absent breath sounds in Infra scapular area.
CARDIOVASCULAR SYSTEM :
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
PALPATION:
Apical impulse is felt on the left 5th intercoastal space 2cm away from the midline.
No parasternal heave, thrills felt.
PERCUSSION:
Right and left heart borders percussed.
AUSCULTATION:
S1 and S2 heard , no added thrills and murmurs heard.
PER ABDOMEN :
INSPECTION:
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
There is no fluid thrill , shifting dullness.
Percussion over abdomen- tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
CENTRAL NERVOUS SYSTEM :
No focal neurological deficits
Sensory and motor systems intact
Normal power , tone and reflexes
INVESTIGATIONS :
COMPLETE BLOOD PICTURE
Haemoglobin 12.1 gm/dl
Total Count 5.700 cells/cumm
Neutrophils 53%
Lymphocytes 35%
Eosinophils 02 %
Monocytes 10%
Basophils 0%
Platelet Count 3.88 lakhs/cu.mm
Smear : Normocytic normochromic
LIVER FUNCTION TESTS :
Total Bilurubin 0.83 mg/dl
Direct Bilurubin 0.20 mg/dl
SGOT(AST) 17 IU/L
SGPT(ALT) 22 IU/L
Alkaline Phosphate 215 IU/L
Total Proteins 6.7 gm/dl
Albumin 3.59 gm/dl
A/g Ratio 1.15
RENAL FUNCTION TESTS :
Urea 17 mg/dl
Creatinine 0.8 mg/dl
Uric Acid 5.6 mg/dl
Calcium 10.2 mg/dl
Phosphorous 3.3 mg/dl
Sodium 138 mEq/L
Potassium 3.8 mEq/L
Chloride 99 mEq/L
COMPLETE URINE EXAMINATIONS :
RANDOM BLOOD SUGAR :
RBS 112 mg/dl
XRAY :
On admission :ULTRASOUND :
LEFT MODERATE TO GROSS PLEURAL EFFUSION WITH COLLAPSE OF UNDERLYING LUNG SEGMENTS
PLEURAL FLUID ANALYSIS :
SUGAR 93
PROTEINS-51
Total count - 1250
Differential count - 90 % neutrophils , 10% leukocytes.
Pleural tap video: https://www.youtube.com/shorts/2Elf1Jyl2sU
PROVISIONAL DIAGNOSIS :
Left sided pleural effusion
TREATMENT :
Medical Treatment:
2/6/22 :
1.02 INHALATION WITH NASAL PRONGS ELITIM
2.INJ AUGMENTIN 1.2GM IV TID
3.INJ PAN 40 MG OD BBF
4.T DOLO 650MG PO SOS
5. SYRUP GRILLINCTUS DX 2 TSP TID
3/6/22 :
1.INJ AUGMENTIN 1.2GM IV TID
2.INJ PAN 40 MG OD BBF.
3.Tab DOLO 650MG PO SOS
4. SYRUP GRILLINCTUS DX 2 TSP TID
4/6/22 :
1.INJ AUGMENTIN 1.2GM IV TID
2.INJ PAN 40 MG OD BBF.
3.Tab DOLO 650MG PO SOS
4. SYRUP GRILLINCTUS DX 2 TSP TID
5.NEBULIZATION WITH MUCOMIST
5/6/22 :
1.INJ AUGMENTIN 1.2GM IV TID
2.INJ PAN 40 MG OD BBF.
3.Tab DOLO 650MG PO SOS
4. SYRUP GRILLINCTUS DX 2 TSP TID
5.NEBULIZATION WITH MUCOMIST
6/2/22 :
1.INJ AUGMENTIN 1.2GM IV TID
2.INJ PAN 40 MG OD BBF.
3.SYRUP GRILLINCTUS DX 2 TSP TID
Interventional procedures :
1/06/22 :
Diagnostic tap was performed 20 mL was aspirated
2/06/22 :
250 mL straw coloured fluid was aspirated
3/06/22 :
1000 mL straw coloured fluid was aspirated
5/06/22 :
20 ml of straw coloured fluid was aspirated
Procedures were uneventful without the occurence of any complications
Advice On Discharge :
1. ATT 4 TABLETS A DAY BEFORE BREAKFAST
2. TAB CEFIXIME 200MG BD FOR 5 DAYS
3. TAB PAN 40 MG PO OD BEFORE BREAKFAST
4. HIGH PROTEIN DIET
5. 2 EGG WHITES PER DAY









.jpeg)
.jpeg)
.jpeg)
.jpeg)
.jpeg)
.jpeg)

Comments
Post a Comment