Bhavani Vegesena
roll no:141
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.( contains information collated by Dr. Durga Krishna PG, Dr.Vamsi PG, Dr. Vilasith intern and from the patient's attender.)
CASE: A 35 year old male , lorry driver by occupation came to the hospital with chief complaints of:
- Cough since 12days
- Fever since 10days
- shortness of breath since 10days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 12days back and then he developed :
- Cough which was non productive in nature and worsened on exertion.
- Fever was insidious in onset and mild. It was intermittent in character which was relieved on taking medication. It was associated with mild body pains.
- Grade 2 dyspnea which worsened overtime.
No H/o of sweating, chills, vomiting, nausea, abdominal pain or burning micturition.
The patient then got tested (RTPCR) for COVID-19 9days back which was declared positive. He might have contracted the virus on his trips in and out of the village owing to his occupation. As advised he was then admitted to hospital 1 on the same day.
He then developed shortness of breath and there was a fall in his oxygen saturation levels 6days back. He was then referred to hospital 2 in the need for oxygen.
HISTORY OF PAST ILLNESS:
K/C/O psoriasis and was treated 8years back.
Not a k/c/o HTN, DM, asthma, CKD, epilepsy.
PERSONAL HISTORY:
DIET: mixed
APPETITE: decreased since the onset of fever
BOWEL AND BLADDER MOVEMENTS: normal
SLEEP: inadequate owing to his occupation
ADDICTIONS: alcoholic ( 3-4 drinks thrice every week)
FAMILY HISTORY:
No significant family history.
GENERAL EXAMINATION:
The patient is moderately built and well nourished.
VITALS:
TEMPERATURE: afebrile
PULSE RATE: 70bpm
BLOOD PRESSURE: 110/70 mm hg
RESPIRATORY RATE: 14 cycles/min
SPO2: 95% on room air
JVP: normal
No icterus, lymphadenopathy, edema.
SYSTEMIC EXAMINATION:
CVS: SI, S2 heard. No murmurs
RS: BAE + , NVBS
ABDOMEN: Soft and non tender. Scars of psoriasis are seen.

CNS: NAFD
INVESTIGATIONS:
COMPLETE BLOOD PICTURE:

INTERPRETATION: decreased lymphocytes.
LIVER FUNCTION TESTS:

INTERPRETATION: increased levels of ALP, , hypoalbuminemia.
RENAL FUNCTION TESTS:

INTERPRETATION: decreased levels of creatinine, uric acid, phosphorus, chloride.
LDH LEVELS:

INTERPRETATION: increased
D-DIMER LEVELS:

INTERPRETATION; increased levels
CHEST XRAY:

INTERPRETATION:
diffuse bilateral consolidation.
PROVISONAL DIAGNOSIS:
Information based on the above investigations is suggestive of viral pneumonia secondary to COVID 19 infection.
TREATMENT:
14/5/2021:
SPO2: 85% on room air
98% with 10L of oxygen
BP: 110/70
- Head end elevation
- O2 inhalation
- Inj Dexa 8mg IV
- Inj clexane 40mg s/c
- Tab MVT
- Tab limcee
- IV fluids- ringer lactate 75ml/hr
15/5/2021:
SPO2: 99% with 10L oxygen
BP: 120/80
continued on the same medications.
16/5/2021:
SPO2: 98% with 10L oxygen
BP: 120/80
continued on the same medications.
17/5/2021:
SPO2: 96% with 2L oxygen
BP: 110/70
continued on the same medications.
18/5/2021:
SPO2: 98% with 4L oxygen
BP: 110/70
continued on the same medications.
19/5/2021:
SPO2: 95% on room air
BP: 110/70
continued on the same medications.
TRP GRAPH CHART:

PNEUMONIA SECONDARY TO COVID-19:The pneumonia that COVID-19 causes tends to take hold in both lungs. Air sacs in the lungs fill with fluid, limiting their ability to take in oxygen and causing shortness of breath, cough and other symptoms.
While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe. Even after the disease has passed, lung injury may result in breathing difficulties that might take months to improve.
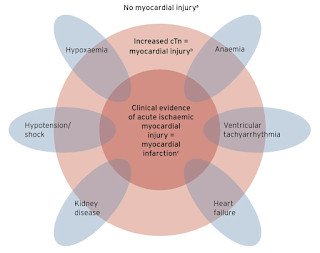
FACTORS EFFECTING LUNG DAMAGE:
- severity of the disease
- associated comorbidities
- treatment given
PREDICTORS OF MORTALITY DUE TO COVID PNEUMONIA:
The following factors were associated with the death of patients with COVID-19 pneumonia :
ALGORITHM FOR RESPIRATORY MANAGEMENT IN COVID 19 PNEUMONIA:
FOLLOW UP IN COVID 19 PNEUMONIA SURVIVORS:
STUDIES :
Efficacy of favipirapir in COVID 19 treatment
Is oseltamivir suitable for fighting against COVID-19:
Blood clots in COVID-19 patients
Pulmonary fibrosis 4 months after COVID-19 is associated with severity of illness and blood leucocyte telomere length
Immunomodulatory therapies for SARS-CoV-2 infection
Note: The information above has been obtained from various sources that I have referenced and acknowledged with their online links and I have paraphrased them further. However the images I have borrowed may have copyright issues as they may not be certified through a creative commons license in which case I hope the original authors will get in touch with me and I shall remove them if they wish.












Comments
Post a Comment