20yr old female with abdominal pain and vomitings
Bhavani vegesena
Roll no 141
Tuesday,March 29, 2022
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CASE PRESENTATION :
A 20 year old female patient, student by occupation has come to the OPD on 22nd March with
CHIEF COMPLAINTS :
1. Abdominal pain since morning 7:00 am (22nd March)
2. Vomiting since morning 7:00 am (22nd March)
HISTORY OF PRESENTING ILLNESS :
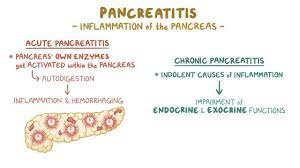
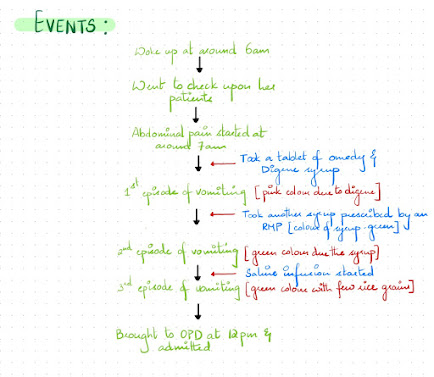
Patient was apparently asymptomatic 5 days back, then she developed abdominal pain in the epigastric region which was sudden in onset, gradually progressive, burning type of pain since morning with no aggravating and relieving factors. For the relief of abdominal pain, she took Omedy and Digene after which she had 3 episodes of vomiting, non projectile, non foul smelling and was relieved by taking medication(zofer). She also has a history of constipation since 2 days.
DAILY ROUTINE:
PAST HISTORY :
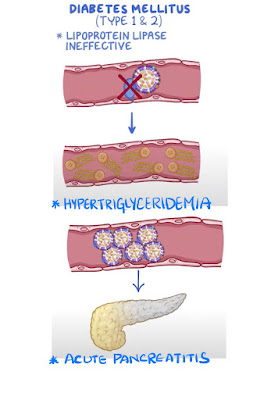
Patient had a history of RTA(fracture to right leg) 3 years back, at the of which she was diagnosed with Diabetes mellitus Type 1 and was prescribed Subcutaneous insulin injection. She took Insulin for 1 year and then
it for 1 month at the end of which her blood glucose levels remained high. So, she continued Insulin. The used oral diabetic medication for a month but as the blood glucose levels remained abnormal, she went back to using Insulin again.
Then she had a history of similar complaint of abdominal pain 6 months back in the epigastric region which was sudden is onset, gradually progressive radiating to left flank and was diagnosed as acute pancreatitis and was treated with conservative management. On further investigations, her blood glucose levels were high and was prescribed subcutaneous Mixtard Insulin (12 units) 2 times a day.
After 10 days, she developed hyperpigmented spots and patches on her lower back and lower limbs for which she consulted the doctor several times but they did not resolve.
She had an irregular lifestyle since the past 2 months and on the night before she complained epigastric pain, she took her Insulin but did not have her meals.
Patient is not a known case of Hypertension, Thyroid disorders, Seizures, Tuberculosis, Asthma.
No history of any blood transfusion, previous surgeries.
PERSONAL HISTORY :
Diet mixed
Appetite decreased
Sleep adequate
Bowel and bladder movements - constipated
No addictions
MENSTRUAL HISTORY :
Menarche at 13 years
Regular cycles, 5/30, Not associated with pains, clots, foul smell.
But she complains of menorrhagia ( spotting) since 1 month.
FAMILY HISTORY :
History of Diabetes mellitus in paternal grandmother.
No similar complaints in the family members.
HISTORY OF ALLERGIES :
No history of any drug or food allergy.
GENERAL PHYSICAL EXAMINATION :
Patient was conscious, coherent, co-operative and well oriented to time, place and person.
Moderately built and nourished.
Pallor, Icterus, Cyanosis, Clubbing, Generalized Lymphadenopathy, Edema are absent.
Vitals :
Temperature - Afebrile
Respiratory Rate - 17 cpm
Pulse Rate : 80 bpm
Blood Pressure - 110/80 mm Hg
SpO2 - 100 % at RA
GRBS - 215 mg/dl
SYSTEMIC EXAMINATION :
Per Abdomen :
On Inspection :
Abdomen appears to be distended and the umbilicus is inverted. Discolouration around umbilicus is seen (Cullen's sign positive)
Multiple scars are seen around the umbilicus.
No sinuses, engorged veins, visible peristalsis, pulsations are seen.
On Palpation :
There is no local rise of temperature.
No tenderness.
No hepatomegaly. No splenomegaly.
No guarding and rigidity.
Percussion :
Tympanic note is heard.
Auscultation :
Bowel sounds are decreased.
CVS : S1, S2 heard. No murmurs.
Respiratory System : Bilateral air entry is present. Normal vesicular breath sounds are heard.
Central Nervous System : Motor and sensory system examination is normal.
INVESTIGATIONS :
1. Lipid Profile :
Elevated Total Cholesterol - 261 mg/dl
Triglycerides - 932 mg/dl
HDL Cholesterol - 81 mg/dl
LDL Cholesterol - 150 mg/dl
2. Glycated Hemoglobin :
HbA1c - 6.9%
3. GRBS :
On day 1 : 265 mg/dl
On day 2 : 222 mg/dl @ 8 am
On day 3 : 215 mg/dl @ 8 am
On day 4 : 243 mg/dl @ 7 am
26.3.22 : 216 mg/dl
4. Urine for Ketone Bodies : Positive
5. Complete Urine Examination :
Albumin : positive
Sugar : positive
6. Urine Protein/Creatinine Ratio :
Spot urine protein : 45.7 mg/dl
Spot urine creatinine : 83mg/dl
Ratio : 0.55
7. Hemogram :
Haemoglobin : 13 g/dl
Total WBC Count : 13,200 cells/cumm
Neutrophils : 79%
Lymphocytes : 15% (decreased)
Eosinophils : 3%
Monocytes : 3%
Basophils : 0
PCV : 39
MCV : 71.4 fl (decreased)
MCH : 23.8 pg (decreased)
MCHC : 33.3%
RDW- CV : 14.2%
RBC Count : 5.46 millions/cumm
Platelet Count : 3.36 lakhs/cumm
8. RFT :
Uric acid - 8.8 mg/dl (2.6-6 mg/dl)
Serum Urea - 29 mg/dl
Serum Creatinine - 0.7 mg/dl
Serum Calcium - 10.2 mg/dl
Na - 137 mEq/L
K - 4.5 mEq/L
Cl - 98 mEq/L
Complete Urine Examination :
Serum Lipase - 135
Serum Amylase - 261
9. LFT
Total Bilirubin - 1.52
Direct Bilirubin - 0.62
AST - 17
ALT - 9
ALP - 181
Total Protein - 6.8
Albumin - 3.37
A/G - 0.98
10. Serum Lipase - 135 IU/L (Elevated)
11. Serum Amylase - 261 IU/L (Elevated)
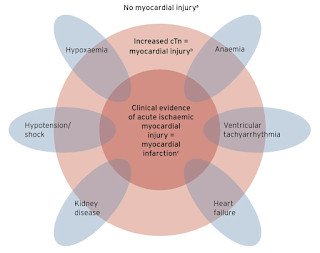
12. ECG
13. 2D Echo


















Comments
Post a Comment