MEDICINE BIMONTHLY ASSIGNMENT - MAY 2021
I have been given the following cases to solve in an attempt to understand the topic of 'Patient clinical data analysis to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
This is the link to the assignment questions:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are the answers to my medicine assignment based on my understanding of the cases:
1) PULMONOLOGY:
A) A 55 year old female patient, with the chief complaints of shortness of breath, pedal edema and facial puffiness.
Patient details: https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
Questions:
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANSWER:
Timeline:
Shortness of breath- 20years ago
(lasting for 1week)
1 episode per year for next 8years
🠋
Shortness of breath- 12years ago
(lasting for 20 days and hospitalized)
1 episode per year
🠋
Generalized weakness - 1month ago
(IV fluids- 3pints in 2days)
🠋
Shortness of breath- 30days ago
(grade 2 SOB)
🠋
Pedal edema- since 15 days
( level: ankle, pitting type)
🠋
Facial puffiness- since 15days
🠋
shortness of breath- since 2days
(grade 4 SOB)
🠋
Drowsiness- since 2days
The patient has a history of working in paddy fields and using indoor chulha since 20years.
The anatomical lesions are generalized to the entire lung bilaterally. 
- tobacco smoking
- air pollution
- indoor burning of biomass fuels
- occupational exposure to dusts, chemical agents
- alpha 1 antitrypsin deficiency
- Facilitate diaphragmatic performance.
- Reduce the risk of mechanical ventilation-associated pneumonia.
- Increase the possibility of more homogeneous alveolar ventilation.
- Reduce the risk of lung injury caused by mechanical ventilation
- May increase the mechanical load against the respiratory system airflow.
- Mechanically ventilated patients
- Meningitis
- Head trauma
- increased intracranial pressure
- Relieving the hypoxia associated with COPD
- Reduces symptoms of dyspnea
- Improved dyspnea and endurance during exercise in COPD patients
- Cardiac output was also increased.
- Hypoxic pulmonary vasoconstriction improved
- Pulmonary hemodynamics may also be improved
- Increased systemic oxygen delivery
- Improved respiratory muscle function
- Stimulate upper airway and facial receptors
- It does not benefit patients with mild to less severe COPD.
- Documented hypoxemia
- respiratory distress
- Increased metabolic demand (burns, multiple injuries, severe sepsis)
- Cardiac failure or myocardial infarction
- Short term therapy (post anesthesia recovery)
"Approximately 75 percent of patients treated with antibiotics were cured, compared with 60 percent of those treated with placebo (number needed to treat = 8; 95% confidence interval, 5 to 27). Additionally, patients taking antibiotics had a longer time to the next exacerbation compared with patients taking placebo (233 versus 160 days)"
Mechanism of action:
Amoxicillin binds to penicillin-binding proteins within the bacterial cell wall and inhibits bacterial cell wall synthesis. Clavulanic acid is a β-lactam, structurally related to penicillin, that may inactivate certain β-lactamase enzymes.
Indications:
Antibiotics should only be started or continued in patients with signs and symptoms of a bacterial infection that include the following:
- Increased dyspnea, increased purulence of sputum, and increased volume of sputum.
- Ventilator support (invasive or non-invasive) for AECOPD.
Patients with a PCT <0.1 ng/mL are unlikely to benefit from antibiotic administration.
"The frequency of exacerbations was 1.48 exacerbations per patient-year in the azithromycin group, as compared with 1.83 per patient-year in the placebo group (P=0.01), and the hazard ratio for having an acute exacerbation of COPD per patient-year in the azithromycin group was 0.73 (95% CI, 0.63 to 0.84; P<0.001)"
Mechanism of action:
Azithromycin binds to the 23S rRNA of the bacterial 50S ribosomal subunit. It stops bacterial protein synthesis by inhibiting the transpeptidation/translocation step of protein synthesis and by inhibiting the assembly of the 50S ribosomal subunit.
Indications:
Antibiotics should only be started or continued in patients with signs and symptoms of a bacterial infection that include the following:
- Increased dyspnea, increased purulence of sputum, and increased volume of sputum.
- Ventilator support (invasive or non-invasive) for AECOPD.
Patients with a PCT <0.1 ng/mL are unlikely to benefit from antibiotic administration.
Study:
- https://www.nejm.org/doi/full/10.1056/nejmoa1104623#:~:text=In%20summary%2C%20we%20found%20that,of%20acute%20exacerbations%20of%20COPD
- https://www.unmc.edu/intmed/divisions/id/asp/clinical-pathways/docs/COPD_pathway2018_Update.pdf
Inj Lasix:
Furosemide decreases peripheral edema and decreases PaCO2 and also increases FEV1 scores when discontinued in patients with COPD as compared to the placebo.
"Ventilation increased from 10.4 L/min (range, 6.7 to 15.4 L/min) at baseline to 11.6 L/min (range, 8.7 to 14.0 L/min) after discontinuation of furosemide (p < 0.05). PaCO(2) decreased from 45 mm Hg (range, 35 to 64 mm Hg) to 41 mm Hg (range, 32 to 61 mm Hg; p < 0.01)"
Mechanism of action:
Furosemide works by blocking the absorption of sodium, chloride, and water from the filtered fluid in the kidney tubules, causing a profound increase in the output of urine (diuresis).
Indication:
patients with stable COPD who satisfied the following criteria:
- Moderate to severe COPD (FEV1 < 70% predicted) with a clinical course consistent with chronic bronchitis and/or emphysema
- Moderate to severe chronic breathlessness (Medical Research Council Dyspnea Scale Grades 4 and 5)
- Age 50 years or older
- https://pubmed.ncbi.nlm.nih.gov/11834646/
- https://www.atsjournals.org/doi/full/10.1164/rccm.200308-1171OC
"Compared with placebo, systemic corticosteroids reduced treatment failure by 46% (95% confidence interval [CI], 0.41 to 0.71), length of hospital stay by 1.4 days (95% CI, 0.7 to 2.2), and improved FEV1 by 0.13 L after 3 days of therapy (95% CI, 0.04 to 0.21). Meanwhile, the risk of hyperglycemia significantly increased (relative risk, 5.88; 95% CI, 2.40 to 14.41)"
- Exacerbations in patients with moderate to severe COPD.
- Should be avoided in stable COPD patients.
"Combined treatment improved QOL and decreased the rate of exacerbation, particularly in patients with an FEV1 of less than 50% predicted (71). Patients with severe COPD may show particular benefit to combined ICS and LABAs as when compared with LABAs alone because patients with an FEV1 of less than 50% predicted had a 35% reduction in moderate and severe COPD exacerbations over a 44-week study period"
Mechanism of action:
Decreases in inflammatory cytokines, C-reactive protein, and inflammatory cells have been observed with corticosteroid use, suggesting a possible mechanism for a therapeutic benefit of steroids.
Indications:
- Acute exacerbation of moderate to severe COPD.
- Stable COPD
- https://www.sciencedirect.com/science/article/abs/pii/S0012369215513366
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2645327/#:~:text=Existing%20evidence%20indicates%20that%20short,stable%20COPD%20is%20not%20recommended.
"In patients with preserved CI (>2.4 L/min/m2) there was an increase of 21.4 ml/min (P = 0.027) (Table 2). There was no increase inV. o2 in patients with mean CI below the group mean. In contrast, patients with a mean CI above the group mean of 3 L/min/m2 showed an average increase of 70.9 ml/min inV. o2 (P < 0.0001)"
Thiamine deficiency impairs production of adenosine triphosphate (ATP), leading to accumulation of adenosine. This increase causes reduction in systemic vascular resistance via direct vasomotor depression, leading to a compensatory high-output state with increased blood volume.
Study:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4298978/
3. What could be the causes for her current acute exacerbation?
- Viral or bacterial infection
- Inhalation of smoke
- Allergy
- Acute symmetrical lesions in thalamus , mamillary bodies , tectal plates , periaqueductal area , floor of 4rth ventricle (includes oculomotor and vestibular nuclei and cerebellar vermis)
- Lesions in the form of vascular congestion, microglial perforation and petechial hemorrhages.
- chronic alcoholism and dependence
- This lead to a chronic thiamine deficiency leading to Wernicke's encephalopathy
- Alcohol dependence lead to symptoms of sweating , restlessness, and seizures as withdrawal symptoms on stoppage of alcohol.
'Patients with suspected WE were treated with ≥500 mg intravenous thiamine for a median of 3 days with 73% of patients (eight out of eleven) displaying symptom resolution or improvement after treatment.'
- patients with severe liver dysfunction.
- patients who are at high risk of experiencing serious medical consequences following sedation
- people with severe lung disease
- elderly patients
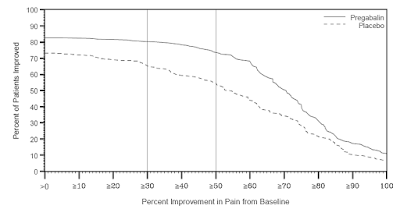
'Alcohol withdrawal symptoms and craving for alcohol resulted significantly reduced (p < 0.001) over time after pregabalin treatment. Pregabalin also resulted in a favourable improvement in psychiatric symptoms and quality of life (p < 0.001).'
- Associated psychiatric symptoms in patients with alcohol withdrawal symptoms
- Seizure prone patients of alcohol withdrawal
- Anxiety, hostility and psychoticism in patients of alcohol withdrawal
- Chronic alcoholics presenting with diabetic ketoacidosis
- Chronic alcoholics presenting in the comatose state
Compared with placebo or no intervention, lactulose significantly reduced the risk of no improvement in neuropsychological tests (RR: 0.52, 95% CI: 0.44–0.62, P<0.00001), the time required for the completion of the number connection test-A (WMD: −26.95, 95% CI: −37.81 to −16.10, P<0.00001), and the mean number of abnormal neuropsychological tests (WMD: −1.76, 95% CI: −1.96 to −1.56, P<0.00001). Furthermore, the meta-analysis also showed that lactulose prevented the progression to overt hepatic encephalopathy (RR: 0.17, 95% CI: 0.06–0.52, P=0.002), reduced blood ammonia levels (WMD: −9.89 µmol/l, 95% CI: −11.01 to −8.77 µmol/l, P<0.00001), and improve health-related quality of life (WMD: −6.05, 95% CI: −6.30 to −5.20, P<0.00001). However, no significant difference was observed in the mortality of patients with MHE (RR: 0.75, 95% CI: 0.21–2.72, P=0.66), and lactulose significantly increased the incidence of diarrhea (RR: 4.38, 95% CI: 1.35–14.25, P=0.01).
In a patient with hypertension due to hypokalemia given with KCl therapy caused an average rise in the serum potassium concentration of 0.56 mmol per liter, the mean blood pressure fell by an average of 5.5 mm Hg (P = 0.004), with at least a 4 mm Hg fall observed in 9 of the 16 patients. The fall in blood pressure correlated with a fall in plasma renin activity (r = 0.568, P = 0.043) but not with changes in plasma aldosterone levels or other variables.
- Alcohol affects the ability of the kidneys to maintain water balance. When alcohol dehydrates the body, the drying effect can affect the normal function of cells and organs, including the kidneys.
- Too much alcohol can also affect blood pressure. High blood pressure is a common cause of kidney disease. More than two drinks a day can increase your chance of having high blood pressure.
- Chronic drinking can also cause liver disease. This adds to the kidney's job. The rate of blood flow to your kidneys is usually kept at a certain level, so that your kidneys can filter your blood well. Liver disease impairs this important balancing act.
c) Primary etiology in causing the disease :
- Hypertension
- Chronic alcoholism
Cochrane Review of randomized controlled trials of betahistine versus placebo in patients with symptoms of vertigo suggested that betahistine may have a positive effect in terms of reduction in vertigo symptoms
- agonist of H1 receptors and
- antagonist of H3 receptors.
"For every 100 patients receiving an adequate dose of ondansetron 20 patients will not vomit who would have vomited had they received placebo. The antinausea effect is less pronounced. Of these 100, three will have elevated liver enzymes and three will have a headache who would not have had these adverse effects without the drug"
There was a significant 14% (SD 7) proportional reduction in mortality during the scheduled treatment period (343 [3·3%] deaths among aspirin-allocated patients vs 398 [3·9%] deaths among placebo-allocated patients; 2p=0·04). There were significantly fewer recurrent ischaemic strokes in the aspirin-allocated than in the placebo-allocated group (167 [1·6%] vs 215 [2·1%]; 2p=0·01) but slightly more hemorrhagic strokes (115 [1·1%] vs 93 [0·9%]; 2p>0·1). For the combined in-hospital endpoint of death or non-fatal stroke at 4 weeks, there was a 12% (6) proportional risk reduction with aspirin (545 [5·3%] vs 614 [5·9%]; 2p=0·03), an absolute difference of 6·8 (3·2) fewer cases per 1000. At discharge, 3153 (30·5%) aspirin-allocated patients and 3266 (31·6%) placebo-allocated patients were dead or dependent, corresponding to 11·4 (6·4) fewer per 1000 in favour of aspirin (2p=0·08).
"Compared with placebo, standard-dose statin treatment resulted in a significant relative risk (RR) reduction of 15% in the occurrence of any major cardiovascular or cerebrovascular event (RR 0.85, 95% CI 0.79–0.91). Compared with standard-dose statin treatment, intensive-dose statin treatment resulted in an additional 9% relative risk reduction (RR 0.91, 95% CI 0.84–0.98)."
- They are aged 40 to 75 years;
- They have 1 or more CVD risk factors (i.e., dyslipidemia, diabetes, hypertension, or smoking);
- They have a calculated 10-year risk of a cardiovascular event of 7.5% to 10%
The CREDO trial, PCI-CURE subset analysis, and ISAR studies support the benefit of early treatment with clopidogrel before PCI. The combined analysis of these studies clearly indicates that adequate inhibition of platelet function with clopidogrel and aspirin alone can be achieved in troponin-negative patients without a need for a Gp IIb/IIIa inhibitor on board.
- Primary prevention of thromboembolism atrial fibrillation
- Symptomatic carotid artery stenosis
- Secondary prevention post-coronary artery bypass grafting
- Peripheral artery percutaneous angioplasty in •peripheral artery bypass grafting
- In conditions of thiamine deficiency commonly noticed in chronic alcoholics with presenting symptoms of Beri Beri and Wernicke's encephalopathy
- In malabsorption disorder caused due to chronic alcoholism
- In patients with chronic alcoholism and associated psychiatric symptoms.
"The crude incidence of stroke was 289/100000 person-year in controlled hypertensive subjects and 705/100000 person-year in treated hypertensive subjects with BP 140/90 mm Hg. It was estimated that 45% of all strokes among subjects with treatment for hypertension might be attributed to uncontrolled BP. HTN is a major risk factor associated with 67%(70.104) of patients with AIS. Multivariate analysis suggests higher odds of 4.088(95%Cl, 0.721–23.179) and 2.437(95%Cl, 0.721–23.179) for 12 and 18 months outcome in patients with AIS and HTN, respectively."
"Most case-control and cohort studies either reported only on total strokes or on a combined group of hemorrhagic strokes including intracerebral as well as subarachnoid hemorrhages. There was a consensus among reports that heavy alcohol consumption was associated with a higher risk of hemorrhagic strokes. Controversy remains regarding the effect of mild-to-moderate alcohol consumption: while some studies reported a protective effect, others found a dose-dependent linear relationship between the amount of alcohol consumed and the risk of hemorrhagic stroke."
- Old age
- Overhead work
- Stress
- medications like diuretics, enema
- inadequate intake of potassium
- transcellular shift of potassium
- renal causes like osmotic diuresis, RTA
Seizures are actually more common after stroke. Statistics show that seizures afflict 22 percent of people who suffer from strokes. They are important to watch out for as they indicate malfunctions in brain activity and cause an altered state of awareness for a stretch of time.
"A total of 78 chronic alcoholics were examined neurologically as well as by electroneurography, myography and posturography. Clinical signs of peripheral neuropathy were detected in 45% of these patients, with electromyographic and neurographic abnormality in 67% and 55% respectively. Clinical signs of cerebellar ataxia were found in 33% of our patients, whereas posturographic measurements of increased sway were recorded in 69%. The posturographic characteristics of cerebellar anterior lobe atrophy were observed in two-thirds of the latter patients. The severity of cerebellar-ataxia did not correlate with the degree of neuropathy. This lack of correlation is interpreted as an indication of different pathogenetic mechanisms acting on peripheral nerves and cerebellum."
"Heavy alcohol consumption demonstrated a strong association with increased nonlobar ICH risk (OR 2.04, p = 0.0003). Heavy alcohol consumption was associated with significant increase in nonlobar ICH risk in black (OR 2.34, p = 0.0140) and Hispanic participants (OR 12.32, p < 0.0001)."
Of the 986 patients with TBI in this study, cerebral infarction was observed in 21 patients (2.1%) within 3 months after trauma. In one retrospective cohort study, the prevalence of cerebral infarction was 1.9%.12) Other studies revealed that prevalence of PTCI was up to 10.4%.19,21,22) These studies included only moderate or severe brain trauma patients. However, patients with TBI of all grades of severity were enrolled in this investigation. Therefore, our result showed low incidence of PTCI compared to other studies. When excluding patient with GCS score of 12 to 15, incidence of PTCI was 6.9%.
Studies have demonstrated a trend toward a higher risk of stroke with lower HDL-C and support HDL-C as an important modifiable stroke risk factor. In patients with recent stroke or transient ischemic attack and no coronary heart disease, only lower baseline HDL-C predicted the risk of recurrent stroke
The main clinical features are localized wasting and weakness of the extrinsic and intrinsic hand muscles, but not accompanied by either sensory loss or spastic quadriparesis. For an accurate diagnosis, attention should be paid to the narrow anteroposterior (AP) canal diameter of the cervical spine (less than 13mm), multisegmental spondylosis in C5-6 and C6-7 disc levels and a reduced transactional area of the spinal cord at the C7, C8, or T1 spinal cord segments.
- Ulnar nerve neuropathy ,
- Cervical myelopathy,
- Upper motor neuron disorders of the cerebral cortex (such as mild hemiplegic stroke or hemiplegic migraine where the same clinical finding has been called the "digiti quinti sign")
- Iron deficiency anemia
|
|
HEART FAILURE WITH PRESERVED
EJECTION FRACTION |
HEART FAILURE WITH REDUCED
EJECTION FRACTION |
|
Risk
factors |
Elderly Females>
males Hypertension Diabetes
mellitus Obesity
|
Male>female Dyslipidemia Smoking Myocardial
necrosis/ inflammation
|
|
Organ
level |
Concentric LV High LV mass/volume |
Eccentric LV Low LV mass/volume |
|
Molecular
level |
Cardiomyocyte hypertrophy Collagenolysis Interstitial
fibrosis Titin
isoform shift to N2B( stiff spring) |
Cardiomyocyte
loss Replacement
fibrosis Titin
isoform shift to N2BA (compliant spring) |
2. Why haven't we done pericardiocentesis in this patient?
- There is no cardiac tamponade in the patient.
- The pericardial effusion is present as a small pocket .
- The effusion was noted to be resolving on its own.[ resolved from 2.4cm to 1.9cm]
- Cardiac tamponade is a class I indication for PC according to the European Society of Cardiology guidelines for management of pericardial diseases.
- A large (>20 mm) pericardial effusion may also be considered for PC (Class IIa recommendation)
- PC is not typically performed when an effusion is noted to be resolving on its own or less invasive methods can be used to make the diagnosis and treat the source of the effusion.
- Diabetes mellitus
- Old age
- Diastolic filling impairment
- Valvular heart disease
- Collapsing left ventricle
- Chronic alcoholic
- Smoking
- Hypertension
- Diabetes mellitus
- Chronic kidney disease
- Obesity
- Anemia of chronic disease
- Inadequate erythropoietin due renal failure ( CKD)
- Nutritional deficiency of iron
- Decreased RBC production ( Chronic alcoholic since 40years)
- Diabetes mellitus ( narrowing of blood vessels leading to decreased perfusion)
- Heart failure (due to lower perfusion and oxygenation in the extremities)
- Anemia ( halt or slow the wound healing stages, which leaves patients more susceptible to other complications such as wound infection.)
- Stage 1: insulin resistance
- Stage 2: prediabetes
- Stage 3: diabetes type 2
- Stage 4: microvascular complications ( retinopathy, nephropathy, neuropathy)
1. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
- Left atrial appendages
- Left atrium
- Pulmonary artery hypertension
- Congestive cardiac failure
- Temporary intravenous inotropic support until resolution of the acute inducing factors or the patient receives more definitive treatment.
- Continuous intravenous form for inotropic support to bridge patients with late-stage heart failure, stage D.
- Short-term for those hospitalized patients with severe systolic dysfunction who present with low blood pressure .
- Decompensated congestive heart failure because of the sympathomimetic effects.
"a trend towards a lower risk of mortality secondary to heart failure with 394 deaths in the digoxin group compared to 449 in the placebo group with a RR of 0.88 (95%CI: 0.77-1.01, P = 0.06). Overall, the number of hospitalizations attributed to worsening heart failure was lower in the digoxin group compared to placebo with a RR of 0.72 (95%CI: 0.66-0.79, P < 0.001)"
- ACC/AHA and ESC guidelines recommendation on the use of digoxin in heart failure with reduced ejection fraction and normal sinus rhythm.
- Digoxin can be considered in combination with a beta blocker and/or nondihydropyridine calcium channel blocker when the ventricular rate is poorly controlled in patients with underlying left ventricular dysfunction.
- Use of digoxin in the acute management of patients who present with acute ST elevation myocardial infarction.
"double-blind trial of dose-adjusted IV unfractionated heparin (Class I) in 225 patients with partial stable carotid and vertebrobasilar distribution stroke.7 This trial showed that there was no difference in death at 7 days between patients who were treated with unfractionated heparin (1/112 [0.89%]) and those treated with placebo (2/113 [1.77%]). Functional activity at 7 days, 3 months, and 1 year also was not significantly different between groups. At 6 months, the proportion of patients who were dead or dependent was identical for the group that received unfractionated heparin and the group that avoided heparin (62.9% in each)"
Mechanism of action:
Heparin is a sulfated polysaccharide with a molecular weight range of 3000 to 30 000 Da (mean, 15 000 Da). It produces its major anticoagulant effect by inactivating thrombin and activated factor X (factor Xa) through an antithrombin (AT)-dependent mechanism. By inactivating thrombin, heparin not only prevents fibrin formation but also inhibits thrombin-induced activation of platelets and of factors V and VIII.
Indications:
- Heparin is used to prevent acute thrombosis after coronary thrombolysis.
- Heparin represents an effective alternative to warfarin for antithrombotic prophylaxis.
"A significant reduction in mortality was observed in favour of the group treated with carvedilol, with an absolute reduction in mortality of 5.7% over a 5 year follow-up period"
- Left ventricular dysfunction
- Hypertension
- Treatment of mild-to-severe heart failure of ischemic or cardiomyopathic origin
"all average monthly INR values were within therapeutic range (2.0-3.0) without differences in the quality of treatment. More than 50% (P = 0.721) as well as >75% (P = 0.714) therapeutic INR values were similar in both groups (Figure 4)."
"significant efficacy was found after 6 to 8 h (relative risk [RR] 1.23, p = 0.022) and at 24 h (RR 1.44, p < 0.001). Efficacy with toresamide was inferior to class Ic drugs for up to 8 h (RR 0.67, p < 0.001) but no difference was seen at 24 h (RR 0.95, p = 0.50)".
Indications:
- edema / fluid overload
- hypertension
- Diabetes type 2
- Hypertension
- Age- 52years
- The aPTT used to be the most commonly used method to monitor the effect of UFH therapy. UFH potentiates the activity of antithrombin and covalently neutralizes thrombin and activated factor X (anti-FXa).
- We regularly monitor the INR of people using anticoagulants in order to balance the risk of excessive bleeding (when the INR is too high, meaning that the blood is too thin) against the risk of clotting or thrombosis (when the INR is too low or the blood is too thick).
- Diabetes mellitus type 2
- Hypertension
- High cholesterol diet
"A significant reduction in mortality was observed in favour of the group treated with metoprolol, with an absolute reduction in mortality of 5.7% over a 5 year follow-up period"
Mechanism of action:
Metoprolol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart.
Indications:
- Left ventricular dysfunction
- Hypertension
- Treatment of mild-to-severe heart failure of ischemic or cardiomyopathic origin
- NSTEMI
- Acute ST-elevation myocardial infarction (STEMI)
- Non–ST-elevation acute coronary syndrome (NSTE-ACS)
- Unstable angina.
- Stable angina.
- Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
- High risk stress test findings.
- Lack of cardiac surgical support.
- Critical left main coronary stenosis without collateral flow from a native vessel or previous bypass graft to the left anterior descending artery.
- Coagulopathy.
- Hypercoagulable states.
- Diffusely diseased vessels without focal stenosis.
ANSWER:
The 2013 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines for the management of STEMI consider primary PCI as a class I indication in STEMI patients within 12 hours’ of initial symptom onset.2 Beyond this timeframe PCI does not show benefit, as shown in the occluded artery trial which evaluated PCI benefit among stable, high-risk patients with persistent total coronary occlusion after MI. The study concluded that PCI performed from 3 to 28 days after MI does not decrease the incidence of death, reinfarction or New York Heart Association (NYHA) class IV heart failure but it is associated with higher rates of both procedure-related and true ST elevation reinfarction.3 A retrospective analysis of the clinical data revealed The Thrombolysis in Myocardial Infarction (TIMI) Risk Score of 4 predicting a 30-day mortality of 7.3% in this patient. Late PCI leads to the increased risks of periprocedural complications, long-term bleeding, and stent thrombosis.
- Smoking
- Diabetes mellitus
- Hypertension
"The major end point, total mortality, was 10.8% in the aspirin group and 9.7% in the placebo group. There was a nonsignificant trend indicating a lower incidence of nonfatal myocardial infarction in the aspirin group (6.3%) compared with the placebo group (8.1%)"
Mechanism of action:
Acetylsalicylic acid (ASA) blocks prostaglandin synthesis. It is non-selective for COX-1 and COX-2 enzymes . Inhibition of COX-1 results in the inhibition of platelet aggregation for about 7-10 days (average platelet lifespan). The acetyl group of acetylsalicylic acid binds with a serine residue of the cyclooxygenase-1 (COX-1) enzyme, leading to irreversible inhibition. This prevents the production of pain-causing prostaglandins. This process also stops the conversion of arachidonic acid to thromboxane A2 (TXA2), which is a potent inducer of platelet aggregation.
Indications:
- Reducing the risk of cardiovascular death in suspected cases of myocardial infarction
- Reducing the risk of a first non-fatal myocardial infarction in patients, and for reducing morbidity and mortality in cases of unstable angina and in those who have had a prior myocardial infarction
- Reducing the risk of transient ischemic attack
- Reduce the risk of non-fatal myocardial infarction.
- Reduce the risk of fatal and non-fatal stroke.
- Reduce the risk for revascularization procedures.
- Reduce the risk of hospitalization for CHF.
- Reduce the risk of angina.
"The primary endpoint of all-cause mortality by hospital discharge was significantly lower in the clopidogrel group (7.5%, n=1,726 vs. 8.1%, n=1,845; p=0.03). Additionally, the co-primary composite endpoint of death, reinfarction, or stroke was lower in the clopidogrel group (9.2%, n=2,121 vs. 10.1%, n=2,310; p=0.002). Reinfarction was lower in the clopidogrel group (2.1% vs. 2.4%, p=0.02), but stroke did not differ by treatment group (0.9% vs 1.1%, p=NS). Any major bleed occurred in 0.58% of the clopidogrel group and 0.55% of the placebo group"
- Use during a percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) and stable ischemic heart disease.
- Primary prevention of thromboembolism atrial fibrillation
- STEMI
- Acute ST-elevation myocardial infarction (STEMI)
- Non–ST-elevation acute coronary syndrome (NSTE-ACS)
- Unstable angina.
- Stable angina.
- Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
- High risk stress test findings
•Moderate left pleural effusion with basal atelectasis with a build-up of fluid between the tissues that line the lungs and the chest.
•Left pneumothorax secondary to broncho pleural fistula. This condition occurs when air leaks into the space between the lungs and chest wall.
- Chronic and excess consumption of alcohol.
There are few randomized clinical trials about the use of antibiotics in AP. Pederzoli et al. in 1993 [16] conducted the first of them, which analyzed 74 patients with SAP in six medical centers in Italy. The patients were randomized in two groups: one control with 33 patients and the treatment group with 41 patients that received Imipenem 3 × 500 mg/day intravenously (i.v.) during 14 days. They observed reduction in pancreatic sepsis in patients that received antibiotics (30.3% vs. 12.2%, p < 0.01). However, they did not find reduction in mortality between the groups (12% vs. 7%, respectively).
It was a prospective randomized double-blind trial that analyzed 114 patients, 58 that received antibiotics (Metronidazole 2 × 500 mg/day i.v.) and 56 that received placebo. It was established that if any patient developed systemic inflammatory response, organic failure, any kind of infection or clinical deterioration, this patient would be discontinued from the protocol with open antibiotic treatment. Their results showed that the use of antibiotics did not reduce pancreatic infection (12% antibiotics vs. 9% placebo, p = n.s.) and mortality (5% antibiotics vs. 7% placebo, p = n.s.). However, 28% of patients in the group that received antibiotics had their protocol opened, versus 46% in the placebo group (p = 0.037). Furthermore, the mean time to open the protocol was 11.5 days in the treatment group and 5 days in the placebo group (Table 2). Based on these data, it is reasonable to suppose that a group of patients had benefits receiving early antibiotics.
Patients with necrotizing pancreatitis suggests that EN may cause complications in patients with ductular damage. In the second week, the patients with acute pancreatitis and enteral route of food administration developed >50% pancreatic necrosis, resulting in gastroduodenal obstruction and pain, leading to the use of TPN being a safer and a recommended option.
The complication rate was lower in the treatment group with regard to sepsis (24% vs 76%, P = 0.0002) and ARDS (28% vs 56%, P = 0.04). The hospital stay was shorter in the treatment group (20.6 vs 33.1 days, P = 0.04). Two patients died in the treatment group and eight in the control group (P < 0.019). These results suggest that octreotide may have a beneficial effect in the treatment of severe acute pancreatitis.
This trial shows that octreotide has no benefit in treatment of acute pancreatitis.
"Mild AP was induced in rats by caerulein (n = 12). Severe AP was induced by infusion of glycodeoxycholic acid (10 mM) into the pancreatic duct combined with caerulein (n = 12). Both AP models were randomized to PPZ treatment (20 mg/kg at baseline and after 12 h) or placebo. Control animals received Ringer solution (n = 6) without AP induction. After 24 h severity of AP was examined by histology, enzyme levels, edema and inflammatory markers (myeloperoxidase, protein profiling). Furthermore, CD62P and CD31 for leukocyte and platelet activation were investigated"
Pain intensities (mean ± SD, 0 = none, 100 = unbearable) before treatment and on day 4 were 75 ± 19 and 8 ± 13 with tramadol (P < 0.001), and 65 ± 21 . On day 4, 67%of patients with tramadol rated their analgesia as excellent (P < 0.001) with mean respective doses of840 mg (range: 80-1920) . OroFecal transit was unchanged after five days of tramadol. Rectal distension threshold pressures increased with tramadol (P < 0.01). It is concluded tramadol is a potent analgesic in severe chronic pancreatitis pain. Tramadol interfered significantly less with gastrointestinal function and was more often rated as an excellent analgesic.
- One is because that sympathetic hyperactivity makes glucagon elevated.
- Secondary, microcirculation disorder makes pancreas edema, ischemia and necrosis, affecting secretion and excretion of insulin. In severe acute pancreatitis, there may be ketoacidosis
- Hyponatremia
- Urinary tract infection
- TURP syndrome
- Dysphagia more to solids initially and later to liquids also
- Hoarseness of voice
- Laryngeal crepitus
- Regurgitation of food
- Cough on consumption of food or liquids
7) INFECTIOUS DISEASE AND HEPATOLOGY:
A) A 55 year old male patient who is a palm tree climber by occupation came on 17th April 2021 with the chief complaints of pain abdomen since one week decrease appetite since one week fever since two days
Patient details : https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
QUESTIONS :
1) Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it? What could be the cause in this patient?
Answer :
Yes , chronic consumption of locally made alcohol might have caused the liver abscess in this patient. Liver abscess is commonly caused due to organisms such as amoeba and other infections. Locally made alcohol is an important predisposing factor for both pyogenic and amebic liver abscess due to the alcoholic effects on the liver
From our study it was undoubtedly proved that alcoholism, mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess
2) What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
Answer :
Reason for the association between local alcohol beverages and ALA could be multifactorial. Factors influencing the association could be related to:
- the pathogen,
- contents of beverages,
- status of the liver, and
- the immunity of the host.
- nutritional status of the population
- poor sanitation
"Alcohol can predispose to ALA through a multitude of mechanisms, including hepatic damage by alcohol, lowered body resistance and suppression of liver function due to poor nutritional status of habitual consumers of alcohol, increased presence of amoebae in the liquor prepared locally with poor regard to aseptic procedures, and depression of immune mechanisms in chronic alcoholics.” A study conducted in India in 2011 showed that 67.5% of patients with amoebic liver abscess are from the low socioeconomic class and 72% were alcoholics. It was also noted that alcoholics had larger abscesses, a greater frequency of complications, and delayed resolution of the abscesses.
All these predisposing factors lead to the causation of pyogenic liver abscess due to amebic infection and other infections of the liver.
References : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077556/
3) Is liver abscess more common in right lobe ?
Answer : Yes , liver abscess is more common in right lobe owing to the fact that it is a more significant part with more blood supply, less commonly in the left liver lobe or caudate lobe.
The usual pattern of abscess formation is that there is leakage from the bowel in the abdomen that travels to the liver through the portal vein. Many cases have an infected biliary tract that causes an abscess via direct contact.
4) What are the indications for ultrasound guided aspiration of liver abscess ?
Answer :
USG guided aspiration of liver abscess is required in:
•Large liver abscess
•Those patients who appear to be superinfected
•Large abscesses impending rupture/ compression signs
•Thin rim of liver tissue around the abscess
•Sero negative abscess
•Failure in treatment following non invasive treatment for 4-5 days
- Age and gender of patient: 21 years ( young ) and male.
- Single abscess.
- Right lobe involvement. ## The abscess is most likely AMOEBIC LIVER ABSCESS … ** But most of the patients with amoebic liver abscess have no bowel symptoms, examination of stool for ova and parasite and antigen testing is insensitive and insensitive and not recommended. # And considering the risk factors associated with aspiration for pus culture: 1) Sometimes ; abscess is not accessible for aspiration if it is in posterior aspect or so. 2) Sometimes ; it has thin thin wall which may rupture if u aspirate. 3) Sometimes ; it is uniquified. ## Due to lack of resources , we cannot confirm whether it is pyogenic / amoebic , so we treat them both empirically in clinical practice.
- an abdominal ultrasound to locate an abscess.
- a CT scan with intravenous contrast, or injected dye, to find and measure the abscess.
- blood tests to look for signs of infectious inflammation, such as an increased serum white blood count and neutrophil level.
A) 50/Male came with chief complaints of fever since 10 days facial puffiness and periorbital edema , weakness of right upper limb and lower limb, altered sensorium.
Patient details : http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
QUESTIONS:
1)What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Answer :
a) Evolution of symptomatology:
Diagnosed with hypertension- 3 years back:
↓
COVID vaccination - 16 days ago
[ fevers, chills and rigors, low grade fever, no diurnal, Following this the patient had similar complaints for the next three days ]
↓
Generalized weakness, facial puffiness and periorbital edema - 10days ago
-Patient was in a drowsy state
↓
Altered state with facial puffiness and periorbital edema- since morning
weakness of upper and lower limbs
b) Anatomical localization of the problem:
The patient mainly presented with facial puffiness and periorbital edema localized to the medial eye canthus of the right eye. The patient also had extreme weakness of upper and lower limb. He also complained of generalized weakness of the whole body and altered/drowsy mental state.
c)Primary etiology of the patient’s problem:
The patient was in an immunocompromised state due to his chronic undiagnosed diabetes mellitus of type 2. Hence this caused him to develop mucormycosis leading to the disease.
The patient also had a chronic hypertension due to which there was a cerebrovascular attack leading to an infarct in his left temporal and frontal lobes.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
Answer :
The pharmacological modalities used are
Itraconazole :
Itraconazole is the only marketed azole drug that has in vitro activity against Mucorales There are case reports of successful therapy with itraconazole alone. However, itraconazole prophylaxis has been described as a risk factor for breakthrough mucormycosis. Therefore, itraconazole should not be considered a first-line agent against mucormycosis, but its use may be considered as adjunctive therapy in selected situations where highly susceptible fungi have been cultured.
Approach as a physician:
Answer:
India is has a high number of diabetics and other immunocompromised patients. During recent times and also in COVID settings the indiscriminate and non judicious use of steroids has increased the number of immunocompromised individuals in the community. This has lead to the vast and sudden increase in the mucormycosis condition in the community which was not a notified disease in the country. This is the main reason for the sudden spike in the cases of mucormycosis in India.
9) MASTER SHEET- COVID 19
https://drive.google.com/file/d/1rBf7kPbRw2tra-Mum0sQnoGrZu-IO81s/view?usp=sharing




























Comments
Post a Comment